
Neuroscience
•
2025-08-05
The gut-brain axis: how your second brain talks to your first
By Dr. Emilė Radytė, CEO of Samphire Neuroscience
When we think about the brain, we often imagine a self-contained control center tucked safely inside the skull. But the brain’s decision-making, mood regulation, and even cravings are influenced by a surprising partner with a lot of buzz - your gut.
This two-way communication, called the gut–brain axis, links the central nervous system with the enteric nervous system (the “second brain” in your gut). And far from being a passive passenger, your gut actively shapes how you think and feel.
Your gut makes neurotransmitters too
You may have heard that neurotransmitters, chemicals like serotonin, dopamine, and GABA, are brain messengers. But your gut produces them too.
In fact, around 90% of the body’s serotonin is made in the gut. While gut-derived serotonin (GDS) doesn’t directly cross into the brain, it can influence brain function indirectly through the vagus nerve, immune signalling, and the hormones that regulate how alert, calm, or motivated you feel.
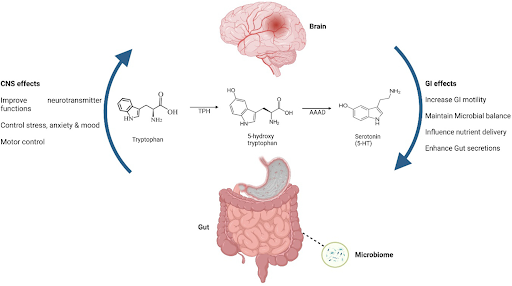
The relationship between your gut and your brain, explained via serotonin pathways, reproduced from Akram et al., 2023 (Food Science and Nutrition)
Meet your microbiome: Billions of “guests” in your gut
Your gut is home to trillions of bacteria, fungi, and other microorganisms, collectively called the gut microbiome. Most aren’t “you” at all; they’re long-term guests whose relationship with your body has evolved over millennia.
These microbes help digest food, train your immune system, and yes, influence your brain and its decisions. They produce compounds like short-chain fatty acids and neurotransmitter precursors that can modulate mood, shape cravings, and even tweak your stress response.
How microbes influence behaviour and cravings
The gut-brain conversation isn’t abstract: it plays out in everyday life.
- Certain bacteria can increase your craving for sugar by producing metabolites that enhance your taste for sweet foods.
- Other microbes produce GABA, a calming neurotransmitter that helps reduce anxiety-like behaviours in animal studies. Read here about how GABA varies in people with PMS/PMDD, and how controlling your nutrition often impacts symptoms by helping interface with the nervous system.
- Some species influence inflammation levels, which can in turn affect mood and cognitive function.
It’s not just your brain telling your gut what it wants; your gut can tell your brain what to want and how to feel.
Bottom-up and top-down control of gut health
Most people think of gut health as something you control from the bottom up: eating probiotic-rich foods, adjusting fiber intake, or taking supplements to “feed” beneficial microbes. And this approach works! Diet is a powerful way to shape the microbiome.
But communication is two-way. Your brain can influence your gut as well. Stress, mood states, and even your belief about what you’re eating can alter gut motility, immune activity, and the chemical messages sent to your brain.
Targeting the brain directly, for example, by strengthening networks that regulate stress and emotional reactivity, can improve gut health from the top down.
Why the gut-brain axis matters for women’s health
For women whose gut symptoms flare alongside hormonal changes, such as endometriosis or polycystic ovarian syndrome (PCOS), this brain-first approach can be a powerful complement to nutritional strategies.
At Samphire Neuroscience, we see the gut–brain axis as a perfect example of why treating the brain and body as separate systems doesn’t work. Your microbiome isn’t just a passenger; it’s an active partner in how you feel, think, and act.
That’s why our work focuses on both sides of the conversation: supporting healthy brain network function through tools like Nettle™, and helping you understand how your lived experiences (stress, mood, diet) shape your gut health in return.
Your brain may be in your head, but in many ways, it’s also in your gut. Learning to listen to both can be the key to feeling your best, and you can track your experiences on Samphire, where we’ll break down what that means for you.
References
Akram, N., Faisal, Z., Irfan, R., Shah, Y. A., Batool, S. A., Zahid, T., Zulfiqar, A., Fatima, A., Jahan, Q., Tariq, H., Saeed, F., Ahmed, A., … [additional authors]. (2023). Exploring the serotonin–probiotics–gut health axis: A review of current evidence and potential mechanisms. Food Science & Nutrition.
Banskota, S., & Khan, W. I. (2022). Gut-derived serotonin and its emerging roles in immune function, inflammation, metabolism and the gut–brain axis. Current Opinion in Endocrinology & Diabetes and Obesity, 29(2), 177–182.
Ridaura, V., & Belkaid, Y. (2015). Gut microbiota: The link to your second brain. Cell, 161(2), 193–194.
Young, E. (2012, December 15). Gut instincts: The secrets of your second brain. New Scientist, 216(2895), 38–42.
Siddiqui, R., Makhlouf, Z., Alharbi, A. M., Alfahemi, H., & Khan, N. A. (2022). The gut microbiome and female health. Biology, 11(11), 1683.
Krog, M. C., Hugerth, L. W., Fransson, E., Bashir, Z., Andersen, A. N., Edfeldt, G., Engstrand, L., Schuppe-Koistinen, I., & Nielsen, H. S. (2022). The healthy female microbiome across body sites: Effect of hormonal contraceptives and the menstrual cycle. Human Reproduction, 37(7), 1525–1543.
Pereira, M. L., Levy, M., Nissapatorn, V., & de Oliveira, G. L. V. (2022). Editorial: Women in microbiome in health and disease 2021. Frontiers in Cellular and Infection Microbiology, 12, 1054190. c

