
PMS,
PMDD
•
2025-08-15
How hormones work for PMDD and PMS
By Dr. Emilė Radytė, CEO of Samphire Neuroscience
Premenstrual dysphoric disorder (PMDD) and premenstrual syndrome (PMS) affect millions of people worldwide. However, the origins of their symptoms are still misunderstood, underdiagnosed, and undertreated. They’re often framed as “hormone problems,” but the truth is more complex, and recent research is finally helping us understand how it all maps together, in order to bring more effective treatments to market.
Theories on the origins of PMDD and PMS symptoms
Over the years, scientists have proposed several possible causes:
- Hormonal fluctuation theory - that symptoms arise because of shifts in estrogen and progesterone during the luteal phase.
- This is still the most popular theory among gynecologists and online, because it’s simple. However, most people with PMS and PMDD have hormone profiles indistinguishable from “healthy” hormone profiles, so for most people this theory leaves more questions than it answers.
- Inflammation theory - that hormonal shifts may activate inflammatory pathways, contributing to pain, fatigue, and mood changes.
- While long-term conditions, such as PMS and PMDD often have some form of inflammatory response, about which we’re just continuing to learn, it again cannot be explained by ‘hormonal shifts’ alone, as every menstruating person’s hormones will need to shift across the menstrual cycle in order to enable ovulation, as shown in the graph below.
- Neurotransmitter theory - that hormonal changes affect serotonin, dopamine, or GABA signalling in the brain.
- This theory is the only one that would explain why different women respond to those same changes in hormones differently, especially at the brain level, where the most distinguishable symptoms of PMS/PMDD, such as low mood, depression, anxiety, indecision, anger arise.
So, it is perhaps surprising that evidence emerging since late 2023 is increasingly pointing to one theory in particular.
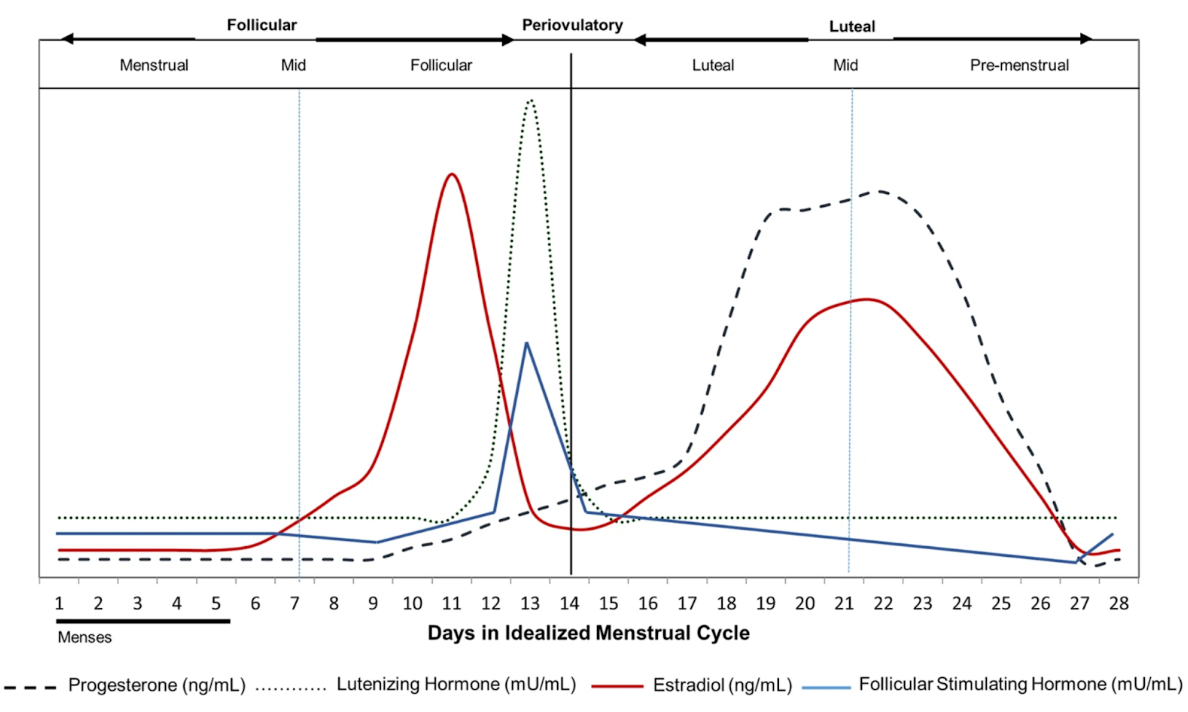
Hormone levels throughout an average menstrual cycle needed to enable regular ovulation and menstruation, reproduced from Draper et al., 2018 (Nature Scientific Reports)
The GABA-progesterone connection and PMDD
Recent clinical and neuroimaging studies are zeroing in on the GABA–progesterone connection. Here’s how it works:
- During the luteal phase, progesterone rises for the vast majority of regularly menstruating women.
- Progesterone is metabolised into a neurotransmitter in the brain, called allopregnanolone (ALLO),
- ALLO is a strong influence on GABA-A receptors,
- GABA is the brain’s main calming neurotransmitter: it regulates mood, anxiety, and emotional processing.
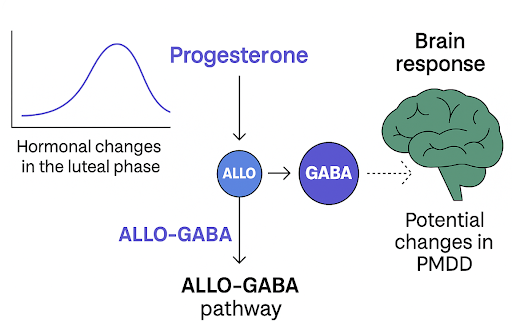
Image showing the impact of progesterone on ALLO, GABA and the ALLO-GABA pathway.
In most people, this hormonal–neurochemical interaction is stabilising. But in PMDD, the brain appears to be very sensitive to ALLO’s effects on GABA, so every cycle, as progesterone rises and more ALLO is produced - the brain’s GABA response is triggered.
WATCH: How PMDD works, explained by Dr. Emilė Radytė
Why this links hormones and the brain for PMDD
This GABA-progesterone model explains something clinicians and people living with PMDD and severe PMS have observed for years: most PMDD symptoms are cognitive and emotional (difficulty concentrating, mood swings, anxiety) functions, all rooted in the prefrontal cortex (frontal lobe) and related brain regions.
So, the emerging evidence suggests that PMDD isn’t caused by “bad” hormone levels. Instead, the brain’s response to otherwise normal hormonal patterns is altered. That’s why most people with PMDD will show “healthy” estrogen and progesterone cycles on lab tests - the difference is in how their brain processes the hormonal signal, and if no one looks at the brain, how would they know?
So, is PMDD a hormonal or brain condition?
The most accurate answer might be: both. The symptoms are triggered by natural hormonal change, but the root lies in neuroendocrine sensitivity - the brain’s unique reactivity to those hormones.
This perspective shifts the focus from trying to suppress or override healthy hormone cycles, something done for years, to supporting the brain in regulating its response.
Where Nettle™ fits in
At Samphire Neuroscience, we design our technology with this science in mind. Nettle™ uses gentle, non-invasive brain stimulation to modulate the neural circuits involved in mood regulation and cognitive control, without altering otherwise healthy hormone levels.
By helping the brain adapt its response to hormonal changes, Nettle™ aims to reduce PMDD symptoms at their neurological source, while leaving the body’s natural cycles intact.
References:
Pritschet et al., Nature Neuroscience (2024) – Hormonal modulation of prefrontal cortex function across the cycle.
Bixo et al., Journal of Neuroendocrinology (2017) – Effects of GABA active steroids in the female brain with a focus on PMDD.
Liu et al., Psychiatry Research: Neuroimaging (2015) – Alterations of GABA and glutamate–glutamine levels in PMDD: A 3T proton magnetic resonance spectroscopy study.
Hantsoo & Payne, Neuroscience & Biobehavioral Reviews (2023) – Towards understanding the biology of PMDD: From genes to GABA.
Stiernman et al., Transcription of GABAA receptor subunits in circulating monocytes and association to emotional brain function in PMDD (2025). PMCID: PMC12287299.
Stiernman et al., Biological Psychiatry (2025) – Emotion generation and regulation in PMDD: Dysregulation of large-scale brain networks across the menstrual cycle.

