
Pain
•
2025-08-15
Why do chronic conditions overlap?
By Kate Ferguson, Chief of Staff at Samphire Neuroscience
I’ve lost count of how many conversations I’ve had where someone tells me about their “main” health condition… and then, almost casually, lists three or four more. The woman with migraines also has endometriosis. The one with fibromyalgia is managing anxiety and IBS. The PMDD patient is juggling ADHD.
It’s not bad luck - it’s multimorbidity, the medical term for living with two or more chronic conditions at the same time. The UK’s National Institute for Health and Care Research (NIHR) calls it one of the most pressing challenges in healthcare today; 1 in 4 adults in England live with two or more chronic conditions.
The UK’s Academy of Medical Sciences has highlighted that biological mechanisms and pathways at the cellular level may trigger other long-term conditions - even when they seem unrelated. While the evidence is still emerging, understanding these shared pathways could change how we prevent and treat chronic illness. Instead of treating each diagnosis in isolation, we could design therapies that address the root causes - improving multiple conditions at once. Sounds simple..?
Why this happens so often in women’s health
When I first learned about multimorbidity, what stood out to me was how rarely current healthcare systems enable doctors to look at the whole picture. We tend to get treated for one diagnosis at a time. You see one specialist for one problem, and another for something else, with no one connecting the dots, or even having the time to.
But for many women, these conditions don’t exist separately. They overlap, influence each other, and often flare at the same time. I’ve seen endometriosis pain trigger bladder and bowel symptoms. I’ve watched premenstrual dysphoric disorder (PMDD) mood changes make attention deficit and hyperactivity disorder (ADHD) brain fog worse (as we explored in When ADHD and PMDD collide). And sometimes, a treatment that helps one condition can make another harder to manage.
From a neuroscience perspective, these overlaps usually trace back to shared biological pathways based in the brain:
- Hormonal sensitivity - In some conditions, the brain and body react more strongly to normal hormonal changes. The drop in progesterone before a period, for example, can trigger PMDD mood changes and worsen joint pain in Ehlers-Danlos syndrome (EDS).
- Neurotransmitter changes - Brain chemicals that carry messages between nerve cells like serotonin, dopamine, and GABA (gamma-aminobutyric acid) all help regulate mood and pain. If one becomes unbalanced, the effects can show up in multiple ways - from anxiety to increased pain sensitivity.
- Central sensitization - This happens when the brain and spinal cord become over-responsive, turning up the intensity of pain and other signals. Once this switch is flipped, it can amplify not only pain, but also fatigue, stress, and mood changes.
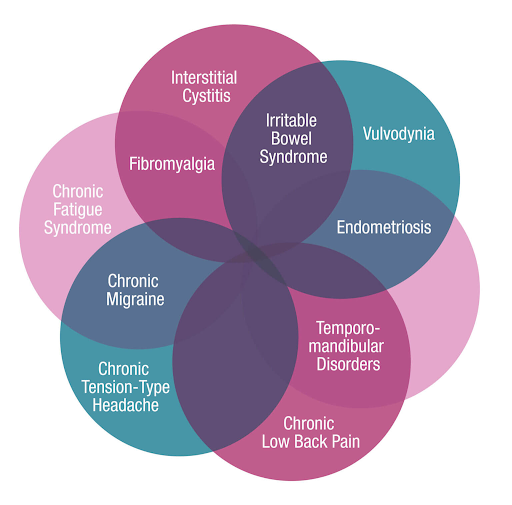
Venn diagram showing overlap of chronic pain conditions including interstitial cystitis, fibromyalgia, irritable bowel syndrome, vulvodynia, endometriosis, temporomandibular disorders, chronic low back pain, chronic migraine, chronic tension-type headache, and chronic fatigue syndrome.
Endometriosis: when pain changes the brain
Endometriosis is often described as a gynecological condition, and whilst that’s how it’s categorized, it’s also a condition that deeply involves the whole body, including the nervous system.
At first, the pain usually follows a monthly pattern. Over time, the nervous system can “learn” the pain and keep it going, even without new inflammation. This is central sensitization in action, with chronic pain and flare-ups as its manifestation. Brain scans have shown changes in the size and connectivity of areas involved in pain processing and emotional regulation.
This matters for multimorbidity because once the nervous system is in a constant state of high alert, it can amplify other signals too - like those from the bladder, bowels, or muscles - making conditions like depression, anxiety, IBS, fibromyalgia, and chronic fatigue more likely to develop alongside endometriosis. In other words, the same nervous system changes that make endometriosis pain persistent can also make you more vulnerable to other chronic conditions.
PMDD: a different kind of sensitivity
PMDD works differently. Hormone levels are normal, but the brain reacts abnormally to the natural hormonal changes of the menstrual cycle.
In the luteal phase (the phase between ovulation and menstruation), the amygdala - the brain’s fear center - becomes more reactive, while the prefrontal cortex - which helps regulate emotions and decision-making - becomes less active. Neurotransmitters like serotonin (linked to mood and well-being) and GABA (which helps calm the nervous system) also become less stable.
This heightened brain sensitivity doesn’t just cause PMDD symptoms - it can intensify other conditions too. Late-luteal ADHD symptoms can worsen (as explored in When ADHD and PMDD collide), sensory overload may spike in autism, and depressive episodes can deepen. Because PMDD affects brain systems that control mood, stress, and pain, it shares pathways with many other chronic conditions, making overlap more common.
Why understanding the overlap matters
On paper, endometriosis and PMDD sound unrelated: one is driven by inflammation and pain, the other by mood and hormonal sensitivity. In reality, they share hormonal timing, nervous system changes, and many of the same companion conditions.
Recognizing these shared pathways changes how we treat them. Instead of managing each diagnosis separately - pain over here, mood over there - we can focus on the underlying systems they have in common: hormone response, neurotransmitter balance, and nervous system regulation.
That matters because it can shorten the path to the right treatment, reduce the trial-and-error of multiple medications, and help address more than one condition at a time.
It’s also why I believe the most effective solutions target the control center - the brain. That’s why Dr. Emilė Radytė created Nettle™, a non-invasive brain stimulation wearable, to work with your nervous system directly. It’s designed to help regulate mood circuits and calm pain pathways, so instead of chasing symptoms one by one, you can address the shared patterns driving them.
References
Bierman, A.S. et al. (2021) ‘Transforming care for people with multiple chronic conditions: Agency for Healthcare Research and Quality’s research agenda’, Health Services Research, 56(Suppl 1), pp. 973–979.
Powell, M. (2021) ‘Making sense of the evidence: Multiple long-term conditions (multimorbidity)’, NIHR Evidence, 30 March.
Rahmioglu, N. et al. (2023) ‘The genetic basis of endometriosis and comorbidity with other pain and inflammatory conditions’, Nature Genetics, 55(3), pp. 423–436.
Smith, S.M. and O’Dowd, T. (2007) ‘Chronic diseases: what happens when they come in multiples?’, The British Journal of General Practice, 57(537), pp. 268–270.
T K Saunders, P. and Horne, A.W. (2025) ‘Endometriosis: new insights and opportunities for relief of symptoms’, Biology of Reproduction, p. ioaf164.

