Endometriosis ,
Pain
•
2024-04-10
The neuroscience of endometriosis
If you’re one of the 1 in 10 women living with endometriosis, you’ll know just how debilitating it can be. The constant, gnawing pain that often makes it hard to get through a day or enjoy the things you love. What’s even more frustrating is that, on average, it takes 6.6 years to get a diagnosis. In some cases, it can take much longer— one UK study reported delays of up to 27 years. And even though endometriosis was first identified in 1860, we still don’t have a clear answer on why it develops.
While traditionally viewed as a gynecological disorder, recent research has revealed a deeper, more complex link between endometriosis and the brain. It turns out that endometriosis isn’t just about where the tissue grows - it’s also about how the brain processes pain. By exploring the neuroscience of endometriosis, we can gain insights into how this condition affects not only the body but also how pain becomes amplified in the central nervous system, transforming a cyclical issue into a chronic, debilitating problem.
How endometriosis pain develops
Initially, endometriosis pain is directly linked to the menstrual cycle and largely cyclical. As the misplaced tissue responds to hormonal fluctuations, inflammation leads to pain signals that are transmitted from the pelvic region to the brain - a process called peripheral sensitisation.
However, for many women, endometriosis pain doesn’t remain limited to the menstrual cycle. Over time, the nervous system adapts, shifting the pain from cyclical to constant. This happens because of central sensitisation, a process where the brain becomes hypersensitive to pain signals - continuing to amplify them, even when the original cause of the pain is less active. What starts as localised inflammation becomes a whole-body problem, with pain spreading to areas like the bladder, bowels, and pelvic muscles.
As the nervous system adapts to this heightened state of pain, neurotransmitters (chemical messengers) go into overdrive, making it difficult for the brain to dampen pain signals. This leads to new symptoms - pain during urination, bowel movements, or sexual intercourse. Anxiety about the pain only makes things worse, leading to a cycle of tension and fear that reinforces the body’s pain response.
Central sensitization: when the brain takes over
So, what exactly is central sensitization? It’s a phenomenon where the central nervous system (CNS) - the brain and spinal cord - becomes overly reactive to pain signals. Even after the initial injury or inflammation subsides, the brain stays on high alert, responding as if the body is still under threat. This constant state of hyperactivity keeps pain receptors firing even without much external input, creating a sense of pain that is disproportionate to the actual stimulus.
A study conducted by Quinta-Marques et al. (2023) found that 100% of endometriosis patients reached the threshold for central sensitization, compared to just 5% of those without the condition. This is a key insight into why endometriosis can lead to such severe chronic pain: it’s not just about the inflammation in the pelvis but about how the brain is interpreting and amplifying these signals.
Explanations as to why those with endometriosis are more likely to have central sensitisation include reduced brain volume in pain-processing regions; increased resting-state connectivity between pain processing regions; and alteration of the hypothalamic-pituitary-adrenal axis (a communication channel between three parts of the brain) leading to reduced capacity to mount a stress response to painful stimuli (McNamara et al., 2021).
Mice models: insights into the brain-pain connection
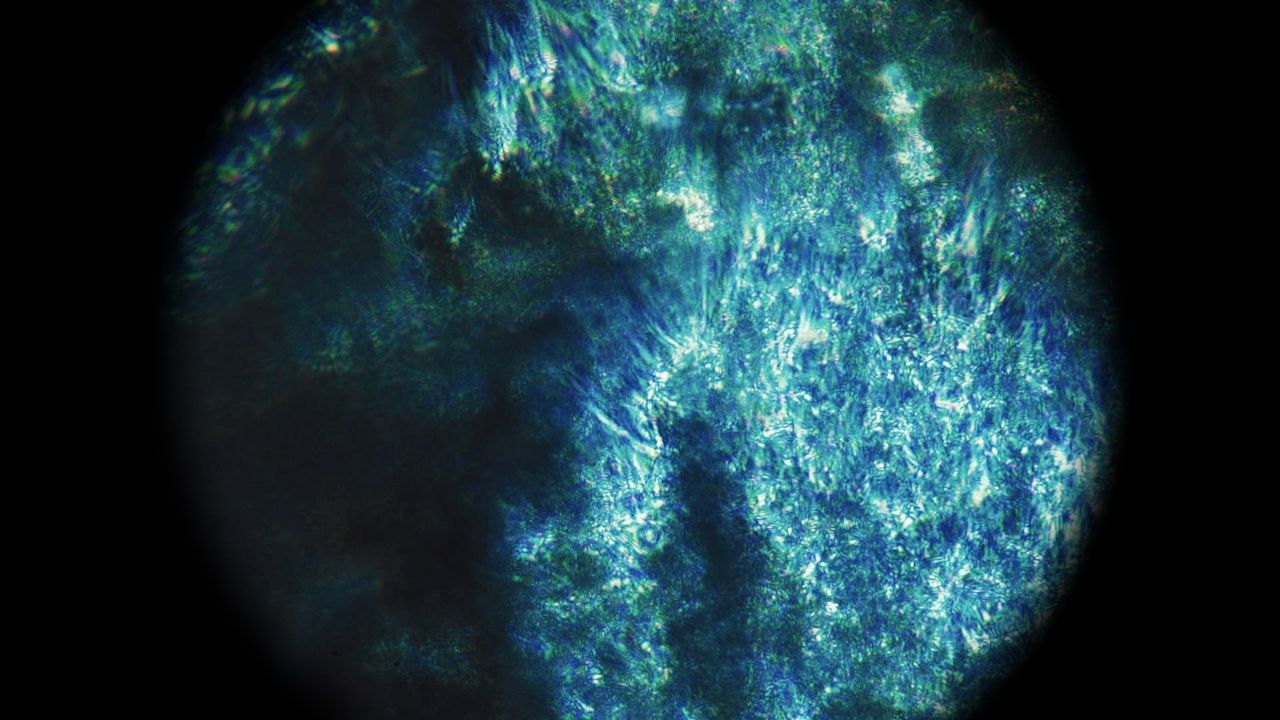
In mice with endometriosis, scientists observed that the condition not only causes physical pain but also alters brain function, leading to central pain sensitization. Repeated input from the inflamed endometriotic lesions activates neuroinflammation, which in turn keeps pain signals flowing to the brain long after the lesions are removed.
The study also uncovered altered neurotransmitter activity in the brain, particularly in the insula, amygdala and hippocampus - regions which regulate both pain and emotions. Specifically, Glutamatergic and GABAergic neurotransmission were found to be dysregulated in mice with endometriosis, potentially leading to the sustenance of chronic pain and emotional dysregulation. This likely explains why many women with endometriosis also experience anxiety and depression. Genes related to pain sensitivity (Gpr88, Glra3) and mood disorders (Lcn2, Nptx2) were also identified, revealing a molecular connection between endometriosis, pain, and mood disorders.
The mental health connection
These findings are often observed symptomatically in humans - for many women, the pain of endometriosis is accompanied by significant mental health challenges. Studies have shown that at least one-third of women with the condition also suffer from psychiatric disorders, such as depression and anxiety.
But the changes aren’t just symptomatic - through neuroimaging studies, researchers have identified structural and functional brain changes in areas related to pain and emotional processing, coining the term "endometriosis brain”. Whilst it’s still unclear whether these changes are driven by chronic pain or endometriosis itself, the connection between the condition and mental health is undeniable, and highlights the importance of treating both the body and the mind when managing endometriosis.
Rethinking pain management: the role of neuromodulation
Given the central role that the brain plays in amplifying pain signals in endometriosis, focusing only on treating inflammation may not be enough. Traditional treatments, such as NSAIDs and hormonal contraception, work to reduce peripheral inflammation, but they often fail to address the central sensitization driving chronic pain. This is where neuromodulation - directly targeting the nervous system - offers a promising alternative.
Studies, including those conducted by us, show the promising potential of transcranial direct current stimulation (tDCS) in the amelioration of pain. In just one cycle, participants in our double-blind, randomized controlled trial experienced a 53% reduction in pain symptoms - an effect likely to improve with sustained use. What’s more - unlike traditional treatments such as hormonal contraception and painkillers, brain stimulation offers a non-invasive, drug and hormone-free option with zero severe side effects (Radytė, 2023).
Therefore, if we begin to reframe pain associated with endometriosis in relation to the brain and central nervous system, it’s not hard to see that brain stimulation has a theoretical advantage when compared with traditional treatments: it directly targets the neural networks involved in both pain perception.
If you or a loved one suffers from menstrual or endometriosis related pain, Nettle™ could help manage symptoms. Order Nettle™ here to benefit from our 90 day trial policy.

