
Neuroscience
•
2025-08-22
Is dopamine really the “happy hormone”?
By Kate Ferguson, Chief of Staff at Samphire Neuroscience
What dopamine really is and how it works
Dopamine is produced in the brain from an amino acid (a building block of proteins) called phenylalanine, transformed through a series of biochemical steps. It communicates through five receptor types (proteins on the surface of cells that receive and respond to chemical signals), D1 to D5, which are found not just in the brain but throughout the body. Depending on which receptors are activated and where, dopamine can motivate us to chase goals, help us learn from experience, fine-tune our movements, and even regulate certain hormones.
Why people call dopamine the “happy hormone”
The nickname comes from dopamine’s role in the brain’s reward system. When you do something pleasurable - whether that’s tucking into your favourite meal, crossing a finish line, or even anticipating a positive outcome - dopamine levels rise in certain brain circuits. One of the most important of these is the mesolimbic pathway, where dopamine-producing neurons in the ventral tegmental area (VTA) send signals to the nucleus accumbens (nAcc). This pathway works closely with the prefrontal cortex, hippocampus, and amygdala, which help us evaluate rewards, form memories, and attach emotional meaning to experiences.
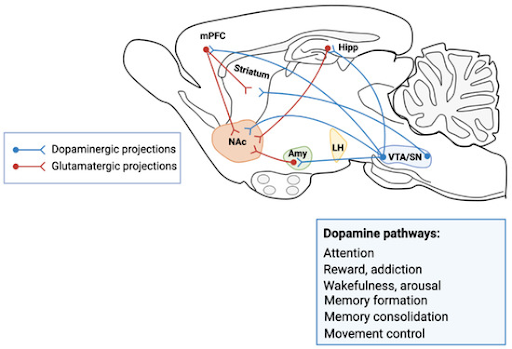
Simplified diagram of the brain’s dopamine reward pathway, showing projections from the ventral tegmental area (VTA) to the nucleus accumbens (nAc), with glutamatergic inputs from the prefrontal cortex, hippocampus, and amygdala. These circuits are central to motivation, reward, and mood regulation. Image adapted from Dopamine: The Neuromodulator of Long-Term Synaptic Plasticity, Reward and Movement Control by Speranza et al., Cells 2021, 10(4), 735;
But dopamine is not happiness itself. It’s more about the wanting than the liking; more about the drive towards the reward than the glow you feel once you’ve got it. It works alongside other neurotransmitters like serotonin, noradrenaline, and GABA to shape our emotional landscape. Too little dopamine in certain brain regions can lead to movement disorders or depression; too much, or poorly regulated signalling, can contribute to impulsivity, addiction, or mood instability.
Dopamine and hormonal changes in women
For women, dopamine’s effects are influenced by hormonal cycles. Estrogen can enhance dopamine production and make its receptors more sensitive, which may explain why many women feel more focused, motivated, or upbeat in the follicular and ovulatory phases of their cycle. Progesterone, which rises after ovulation, can temper dopamine activity in some brain circuits, potentially contributing to the mood changes, dips in motivation, or brain fog that are common in the luteal phase.
Brain imaging in primates has shown that dopamine receptor availability changes across the menstrual cycle, with D2 receptors more available in the luteal phase compared to the follicular phase. This shifting responsiveness helps explain why mood, energy, and even pain perception can vary so noticeably month to month.
Dopamine’s role in PMS, PMDD, pain, and cognitive function
These changes aren’t just theoretical. In PMS and PMDD, atypical sensitivity to hormonal fluctuations can disrupt dopamine’s role in mood regulation, intensifying irritability, low mood, or reduced motivation. Dopamine is also involved in how we process pain, influencing pathways that modulate discomfort - highly relevant in conditions like primary dysmenorrhea and endometriosis, where pain is amplified by the brain’s central nervous system.
Because dopamine is tied to cognitive performance, its ebb and flow across the cycle can influence concentration, decision-making, and reaction time. This makes it not just a chemical of reward, but a key player in how we function and feel day to day.
How brain-based solutions work with dopamine
At Samphire Neuroscience, we begin with the understanding that the menstrual cycle is as much a brain event as a hormonal one. The way your cycle feels - emotionally, mentally, and physically - depends on how your brain interprets and responds to those hormonal changes. That’s why technologies like Nettle™ target regions such as the dorsolateral prefrontal cortex, working with the brain’s own circuitry to support emotional stability, cognitive clarity, and symptom relief, without the systemic side effects of drugs or hormones.
References
Czoty, P.W. et al. (2009) ‘Effect of Menstrual Cycle Phase on Dopamine D2 Receptor Availability in Female Cynomolgus Monkeys’, Neuropsychopharmacology, 34(3), pp. 548–554.
Franco, R., Reyes-Resina, I. and Navarro, G. (2021) ‘Dopamine in Health and Disease: Much More Than a Neurotransmitter’, Biomedicines, 9(2), p. 109.
Gudipally, P.R. and Sharma, G.K. (2025) ‘Premenstrual Syndrome’, in StatPearls. Treasure Island (FL): StatPearls Publishing.(Accessed: 15 August 2025).
Modzelewski, S. et al. (2024) ‘Premenstrual syndrome: new insights into etiology and review of treatment methods’, Frontiers in Psychiatry, 15.
Speranza, L. et al. (2021) ‘Dopamine: The Neuromodulator of Long-Term Synaptic Plasticity, Reward and Movement Control’, Cells, 10(4), p. 735.

