Neuroscience
•
2025-08-22
How does the brain control hormones?
By Dr. Emilė Radytė, CEO of Samphire Neuroscience
Hormones shape so much of our lives - from our energy levels and mood to our menstrual cycles, fertility, and long-term health. But most people don’t know: every hormone in the body starts with a signal from the brain.
Hormones are personal but similar
Hormone levels and patterns vary greatly between people. While we often talk about “average” hormone levels, there’s no one-size-fits-all profile. For women and people assigned female at birth, hormones like estrogen and progesterone follow highly specific patterns and cycles that change across the month in order to enable healthy menstruation, fertility and menopause.
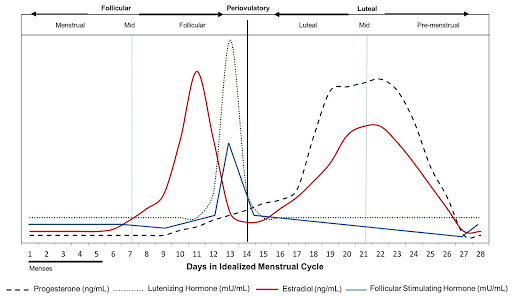
Hormone levels throughout an average menstrual cycle, reproduced from Draper et al., 2018 (Nature Scientific Reports)
And these patterns shift over a lifetime. Your hormonal profile will differ depending on your age, whether you’ve been pregnant, the number of pregnancies you’ve had, and life stages such as perimenopause or menopause. Circumstances like chronic stress, illness, or lifestyle factors can also influence hormonal rhythms.
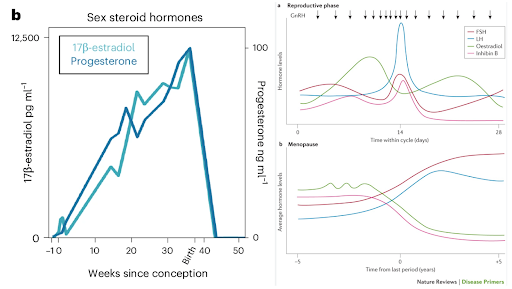
(Left) Hormone levels throughout an average pregnancy cycle, reproduced from Pritschet et al., 2024 (Nature Neuroscience). (Right) Hormone levels throughout an average perimenopause cycle, reproduced from Davis et al., 2015 (Nature Reviews)
The Hormones’ Boss? The Brain
All hormones are produced only after receiving a signal from the brain. The hypothalamus - a small but powerful brain region - is the one you should remember the most. It sends chemical messages to the pituitary gland, which then instructs your ovaries, adrenal glands, thyroid, and other hormone-producing organs to make precise amounts of hormones.
For example, to produce estrogen or progesterone, the hypothalamus releases gonadotropin-releasing hormone (GnRH). This tells the pituitary to release luteinizing hormone (LH) and follicle-stimulating hormone (FSH), which in turn stimulate the ovaries to produce estrogen and progesterone in finely tuned cycles.
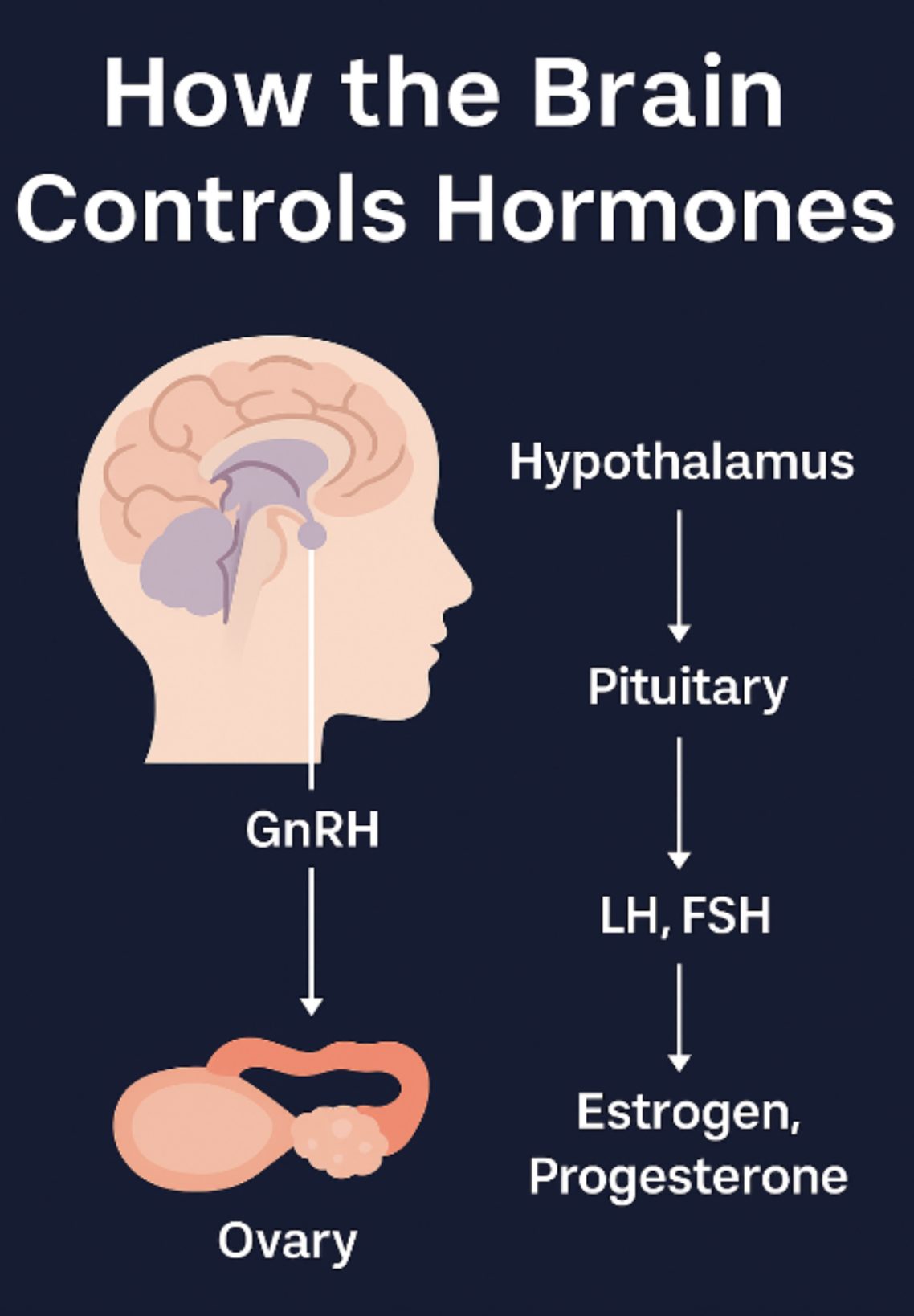
Infographic showing how the brain acts to produce estrogen and progesterone.
To make it clear - no ovarian hormones (progesterone and estrogen) are produced if the hypothalamus (in the brain) does not give the correct signal (GnRH) to the ovaries.
These cycles are not random: they are orchestrated according to feedback from the body, ensuring balance. So, if the body already has a lot of estrogen, whether it’s produced naturally or not, the brain will receive a signal that there is enough estrogen, and won’t release signals to produce more, which in some cases could lead to estrogen dysregulation.
So, What About Those ‘Out of Balance’ Hormones?
It’s common to hear about “hormonal imbalances” in conditions like PMDD, PCOS, or perimenopause, especially when trying to convince people living with those conditions that the solution lies in “fixing” their hormones either by hormonal supplementation or vitamins that are supposed to “regulate” hormones.
In many cases, however, it’s not the hormone-producing glands that malfunction first - it’s the brain’s signalling system that shifts. The hypothalamus or pituitary may change the intensity or timing of the signals, leading to different amounts of estrogen, progesterone, cortisol, or other hormones in circulation.
That’s why thinking about hormones purely at the level of the ovary, thyroid, or adrenal gland is incomplete. Every hormonal change starts in the brain, and the “fix” should usually start there, too.
Why This Matters for Your Health
When we think about treatments for hormone-related conditions - whether it’s menstrual pain, mood changes, or perimenopausal symptoms - we need to consider the brain’s role. Approaches that support healthy brain signalling can, in turn, help restore balanced hormone patterns, by helping your body balance itself out once its “control system” is back on track.
For those whose symptoms are strongly tied to hormonal rhythms, such as premenstrual mood changes or cycle-linked anxiety and pain (dysmenorrhea), Nettle™ offers a way to act at the source. Using gentle, non-invasive brain stimulation, Nettle engages the prefrontal and motor cortex in the brain to support the brain’s response to ever-changing hormones, without altering otherwise healthy hormone production.
At Samphire, our focus is on the neuroscience of women’s health - because to truly understand and improve hormonal wellbeing, we need to start where hormones start: in the brain.
References:
Draper, C.F., Duisters, K., Weger, B. et al. Menstrual cycle rhythmicity: metabolic patterns in healthy women. Sci Rep 8, 14568 (2018).
Davis, S., Lambrinoudaki, I., Lumsden, M. et al. Menopause. Nat Rev Dis Primers 1, 15004 (2015).
Pritschet, L., Taylor, C.M., Cossio, D. et al. Neuroanatomical changes observed over the course of a human pregnancy. Nat Neurosci 27, 2253–2260 (2024).
López, M., & Tena-Sempere, M. (2015). Estrogens and the control of energy homeostasis: A brain perspective. Trends in Endocrinology & Metabolism, 26(8), 411–421.
Martini, L., Motta, M., Piva, F. et al. LHRF, LHRH, GnRH: what controls the secretion of this hormone?. Mol Psychiatry 2, 373–376 (1997).
Murray, C. M., & Orr, C. J. (2020). Hormonal regulation of the menstrual cycle and ovulation. In A. K. H. MacLennan & J. M. K. Reynolds (Eds.), Maternal-fetal and neonatal endocrinology: Physiology, pathophysiology, and clinical management (pp. 159–167). Academic Press.
Wickramasuriya, N., Hawkins, R., Atwood, C., & Butler, T. (2022). The roles of GnRH in the human central nervous system. Hormones and Behavior, 145, 105230.
Lai, W., Li, X., Zhu, H., Zhu, X., Tan, H., Feng, P., Chen, L., & Luo, C. (2020). Plasma luteinizing hormone level affects the brain activity of patients with polycystic ovary syndrome. Psychoneuroendocrinology, 112, 104535.

